Congenital Heart Disease In Children
All SpecialityPage Navigation
ABSTRACT
Congenital heart disease (CHD) is the most common congenital disorder in neonates.
A number of factors including genetic factors, teratogenic exposure and several other unrecognised factors have been associated with its development.
Ventricular Septal Defect (VSD) is the most common type.
INTRODUCTION-
Congenital Heart Defects are structural abnormalities of heart and/or great blood vessels during fetal development.
CHDs account for about 28% of all congenital anomalies. It is a result of lack of normal development of heart during the embryonic phase.
Prevalence- 1% births in the United States.
1.5-1.7/1000 live births in India.
ETIOLOGY –
Mostly unknown.
Sometimes associated with –
• Chromosomal abnormalities and Genetic disorders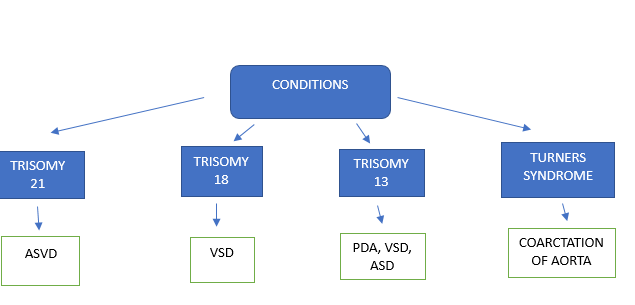
• Teratogenic factors including maternal smoking, alcohol abuse, exposure to retinoid, indomethacin, tocolytics.
• Maternal infection with rubella.
• Additionally, history of epilepsy in mother, phenylketonuria, maternal age above 30, Type 1 and Type 2 DM as well as positive family history are other risk factors.
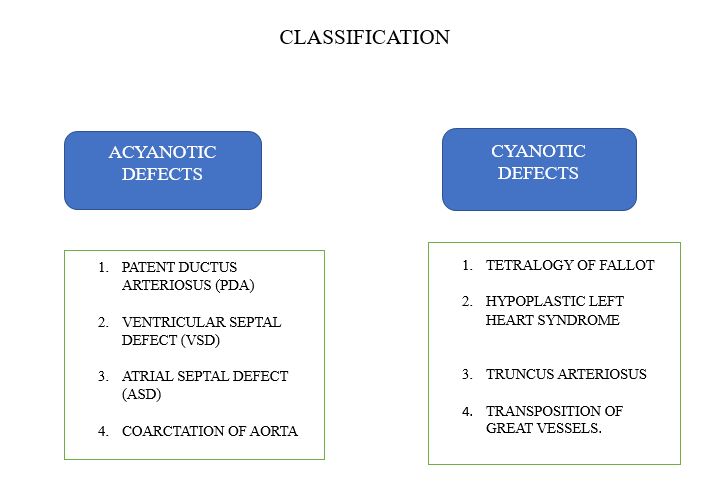
ASD –
• Abnormal opening in the septum between right and left atrium.
• Normally L to R shunt.
• Most common type is secundum ASD (80%).
• Wide fixed split s2 is the pathognomic for ASD.
• Clinical manifestations are non-specific.
VSD –
• Defect in interventricular septum.
• Shunting of blood from L to R.
• Most common type is peri membranous.
• Holosystolic/ high pitched murmur
• Small VSDs are usually asymptomatic. Moderate VSDs can cause frequent respiratory infections and fatigue.
• Larger VSD can lead to reversal of shunt in Eisenmenger syndrome.
TETRAOGY OF FALLOT –
• 4 Defects are present in the heart
1) Right ventricular outflow obstruction
2) Right ventricular hypertrophy
3) Overriding aorta
4) Ventricular septal defect
• Clinical manifestations include cyanosis, tachypnoea, “tet spells”
• Harsh systolic ejection murmur (best heard at left sternal border)
• Boot shaped heart on CXR.
• Surgical repair definitive
COARCTATION OF AORTA –
• Narrowing of the descending aorta typically located at the insertion point of the ductus arteriosus, just distal to the left subclavian artery
• Often associated with bicuspid aortic valve and turners syndrome
• Posterior rib notching and figure 3 sign on CXR.
PATENT DUCTUS ARTERIOSUS –
• Condition in which ductus arteriosus (small artery which connects fetal pulmonary artery to aorta) remains patent and does not close after birth.
• Epidemiology –
1. Prematurity
2. 2:1 female predominance
3. Higher altitude
4. Congenital rubella
• Caused from continual prostaglandin E1 production
• Continuous machine-like murmur and bounding peripheral pulses on physical exam.
PREVENTION –
Prevention of congenital anomalies is important as the impact can be for life. Environmental factors known to be the risk factors in etiology need to be suitably addressed. First approach should be for families with children or relatives with CHD. Second, environmental factors need to be suitably addressed.
DETECTION AND DIAGNOSIS-
Early detection is desirable. The suspicion of CHD is mainly clinical. Evaluation should be done on the basis of Nadas’ criteria for diagnosis of CHD.
The major criteria include -
1. Systolic murmur grade 3 or more
2. Diastolic murmur
3. Cyanosis
4. Congestive cardiac failure
The minor criteria include –
1. Abnormal echo
2. Abnormal X ray
3. Abnormal BP
Presence of 1 major or 2 minor criteria indicates heart disease.
In infants, feeding difficulties are common. Others include poor weight gain, irritability, breathing difficulty, inappropriate sweating and persistent cough.
Read more such content on @ Hidoc Dr | Medical Learning App for Doctors
Recommended News For You
Recommended Articles For You
Featured News
Featured Articles
Featured Events
Featured KOL Videos
1.
Tumor infiltration of major blood vessels, not metastasis, may be primary cause of cancer death
2.
The Predictive Power of Liquid Biopsy in Colon Cancer Outcomes Is Inconsistent.
3.
Research identifies nearly 200 potential breast carcinogens in food packaging materials
4.
Anticoagulation for 12 months has been found to improve outcomes in cancer patients with minor blood clots.
5.
Doxorubicin-Trabectedin Strategy Boosts Survival in Challenging Sarcoma
1.
CAR T + Ibrutinib in R/R Mantle Cell Lymphoma: Phase 2 TARMAC Study Insights
2.
Uncovering the Hidden Symptoms of Parathyroid Cancer in Women
3.
Survivin as a Key Regulator in Gynecological Cancers: Therapeutic and Prognostic Implications
4.
The Basics of Langerhans Cell Histiocytosis: Understanding a Rare Disease
5.
Oncology Trials Roadmap: From Drug Discovery to Delivery and Patient Access
1.
International Lung Cancer Congress®
2.
Genito-Urinary Oncology Summit 2026
3.
Future NRG Oncology Meeting
4.
ISMB 2026 (Intelligent Systems for Molecular Biology)
5.
Annual International Congress on the Future of Breast Cancer East
1.
Understanding the causes of anemia in adults beyond nutritional deficiencies
2.
An Intro to The Multifaceted Advantages of CDK4/6 Inhibitors in HR+/HER2- Advanced Breast Cancer Clinical Studies.
3.
Evolving Space of First-Line Treatment for Urothelial Carcinoma- Case Discussion
4.
An Eagles View - Evidence-based discussion on Iron Deficiency Anemia- Important Points to Know
5.
Revolutionizing Treatment of ALK Rearranged NSCLC with Lorlatinib - Part II
© Copyright 2026 Hidoc Dr. Inc.
Terms & Conditions - LLP | Inc. | Privacy Policy - LLP | Inc. | Account Deactivation

